What is systemic lupus erythematosus?
Systemic Lupus Erythematosus (SLE) is a systemic autoimmune disease that mainly affects young women. The male-to-female ratio is approximately 1:7 to 1:9, with an average onset age of about 20 to 40 years.
Causes of Systemic Lupus Erythematosus
The exact cause of lupus remains unclear, but the medical community knows that factors such as immune system dysregulation, genetics, hormones, and environmental triggers may induce the disease.
Genetic Factors: A family history of lupus increases the risk, and certain gene mutations may be involved.
Environmental Factors: Ultraviolet radiation, certain medications (e.g., anticonvulsants), or viral infections can trigger or worsen the condition.
Hormonal Factors: Estrogen or related hormonal influences are associated with lupus.
Immune System Dysregulation: Autoantibodies attack the body’s own tissues, leading to inflammation and organ damage.
Types of Lupus
Systemic Lupus Erythematosus (SLE): The most common form, affecting multiple systems including joints, skin, kidneys, etc. Symptoms may include fever, joint pain, skin rashes, fatigue, hair loss, and abnormal kidney function.
Discoid Lupus Erythematosus (DLE): Primarily affects the skin, presenting as red, disc-shaped lesions with slightly raised edges that may scab and damage hair follicles. Usually appears on the face, scalp, or ears and worsens with sun exposure.
Drug-Induced Lupus: Caused by certain medications, often after long-term use of drugs such as some antibiotics or antihypertensives. Symptoms resemble SLE but typically improve after stopping the medication.
Others:
- Neonatal Lupus (NLE): Rare, affects newborns, possibly transmitted from mother; features skin rash, arthritis, and heart problems.
- Subacute Cutaneous Lupus Erythematosus (SCLE): Affects the skin with symptoms similar to SLE but usually milder.
- Lupus Panniculitis: Affects subcutaneous tissue, leading to subcutaneous nodules.
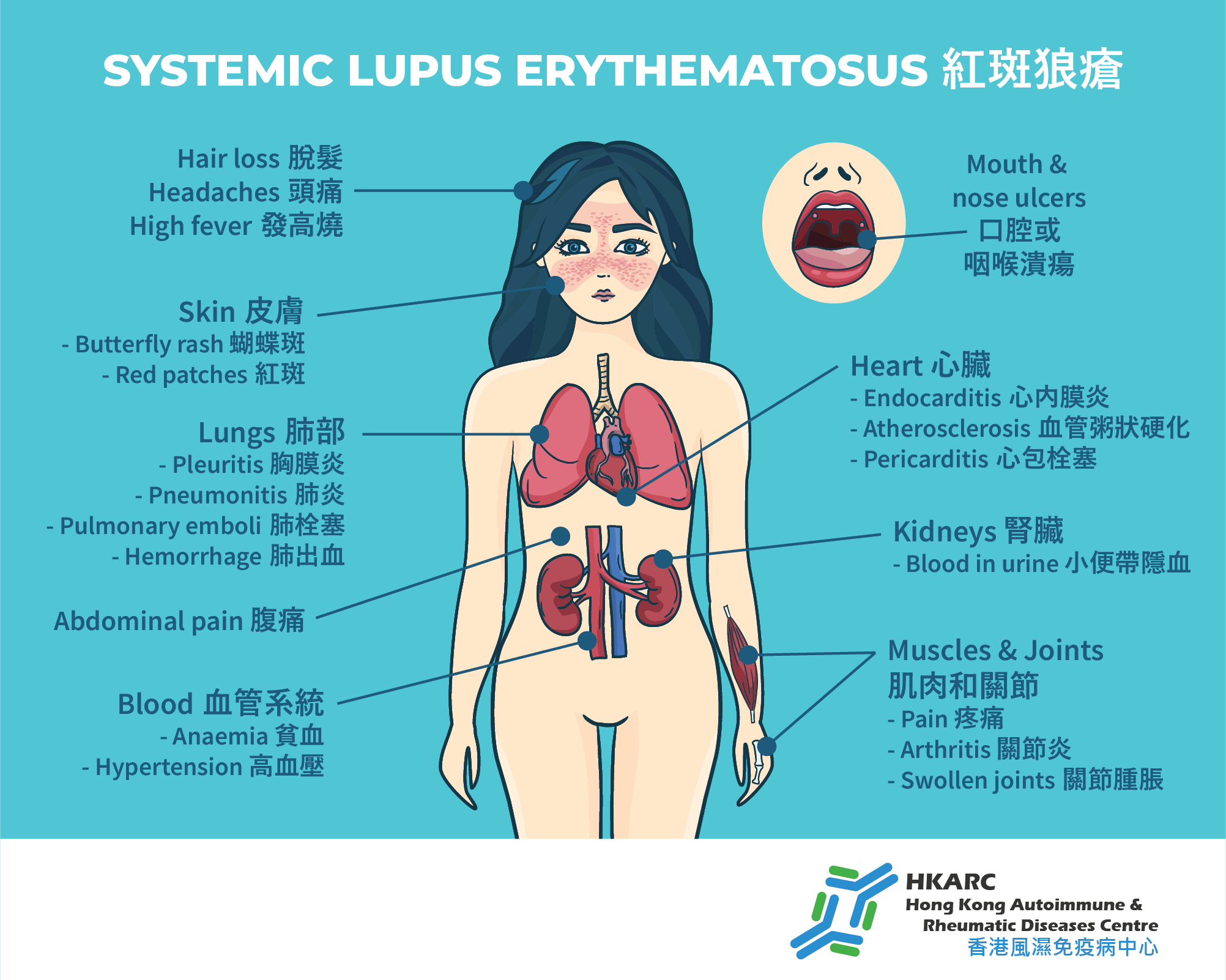
Symptoms of Lupus
Lupus is a chronic disease that can involve various parts of the body. Symptoms are diverse and may include:
- Skin rashes, often butterfly-shaped on the face, but can also appear on fingers, ears
- Arthritis
- Mouth ulcers
- Hair loss
- Fatigue and fever
- Muscle pain or myositis
- Serositis, including pleuritis and pleural effusion
- Hematological abnormalities, such as anemia, leukopenia, thrombocytopenia
- Nephritis
- Neurological and psychiatric issues, such as seizures, cognitive disturbances
In addition to clinical symptoms, blood tests often reveal abnormalities, such as the presence of antinuclear antibodies (ANA), anti-dsDNA antibodies, and usually decreased levels of complement proteins C3 and C4. The diagnosis of lupus is made based on a combination of clinical presentation and laboratory findings, as different patients show varied symptoms.
Complications of Systemic Lupus Erythematosus
Lupus nephritis is one of the most critical complications, which can lead to end-stage renal failure and pose a life-threatening risk. Sometimes, kidney involvement may be asymptomatic, presenting only as fatigue and increased urination, so even mild joint or skin issues should not be ignored. Early consultation with a rheumatologist is advised if lupus is suspected.
Lupus can affect many organs and systems, leading to:
- Neurological issues like headaches, dizziness, behavioral changes, strokes, or seizures
- Hemolytic anemia and thrombocytopenia
- Cardiovascular problems such as pericarditis, myocarditis, and pulmonary issues like pneumonia, pleural effusion
- Other organ damages
Treatment Options
Biologics
Recent guidelines from the European League Against Rheumatism (EULAR) recommend reducing or discontinuing corticosteroids in active lupus cases and adding biologic therapies to help control inflammation. Biologics target active immune factors, reducing cell proliferation and the production of destructive antibodies, thereby protecting organs like the kidneys. Use of biologics can also lower steroid doses, helping to manage lupus nephritis effectively and reduce the risk of disease progression or flare-ups.
Corticosteroids
Corticosteroids have anti-inflammatory and immunosuppressive effects, effectively reducing inflammation and preventing immune-mediated tissue damage. They are essential in managing rheumatic diseases but long-term use may cause side effects such as infections, osteoporosis, avascular necrosis, and cataracts.
Traditional Disease-Modifying Anti-Rheumatic Drugs (DMARDs)
These drugs gradually replace corticosteroids in controlling autoimmune activity, reducing joint inflammation and damage, alleviating pain, swelling, and stiffness, and slowing disease progression. Different DMARDs are chosen based on the organs involved.
Antimalarial Drugs
Antimalarial Drugs Medications like hydroxychloroquine are commonly used in autoimmune diseases to reduce disease activity. When combined with corticosteroids, they can lower steroid doses and side effects. Hydroxychloroquine also has anti-inflammatory and immune-modulating properties.
FAQs
• Is Lupus contagious?
No. Lupus is an autoimmune disease and is not infectious, so it cannot be transmitted from person to person.
• Can Lupus be cured?
Currently, there is no cure for lupus. However, it can be managed effectively with medications and lifestyle adjustments to reduce the risk of permanent organ or tissue damage. While not curable, modern treatments enable patients to lead normal lives and prevent serious complications.
• How is Lupus different from Eczema?
Lupus often begins with facial skin involvement, presenting as a butterfly-shaped rash on the cheeks, usually without itching. It can also cause fever, mouth ulcers, hair loss, and may affect joints, as well as the heart, brain, and kidneys. Eczema or dermatitis usually causes intense itching and can appear anywhere on the body, with symptoms predominantly characterized by itching and skin inflammation.