What is Ankylosing Spondylitis?
Ankylosing Spondylitis (AS) is an autoimmune disease. About 2-3 out of every 1,000 people are affected by this condition. The average age of onset is between 17 and 40 years old. The male-to-female ratio is approximately 3:1.
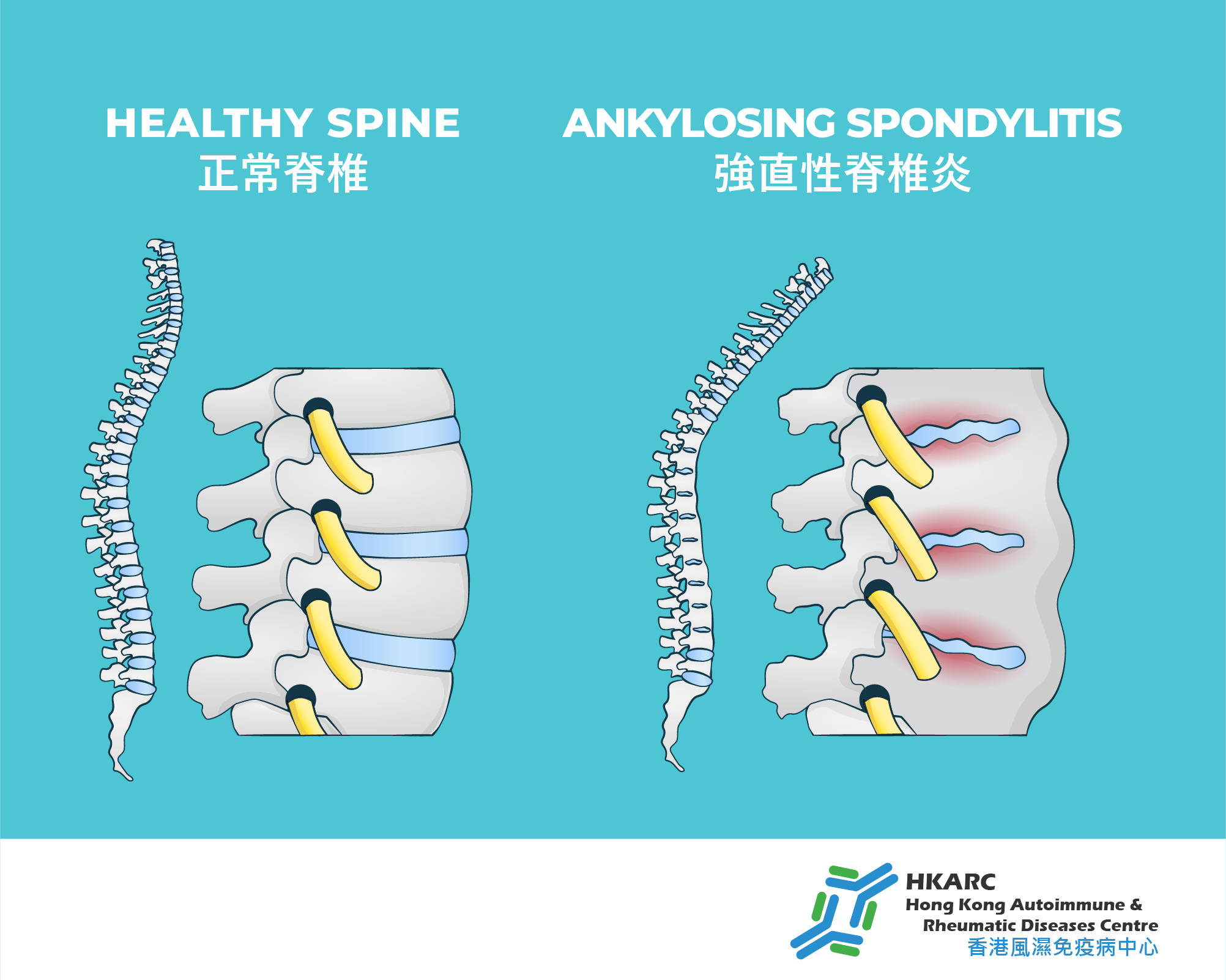
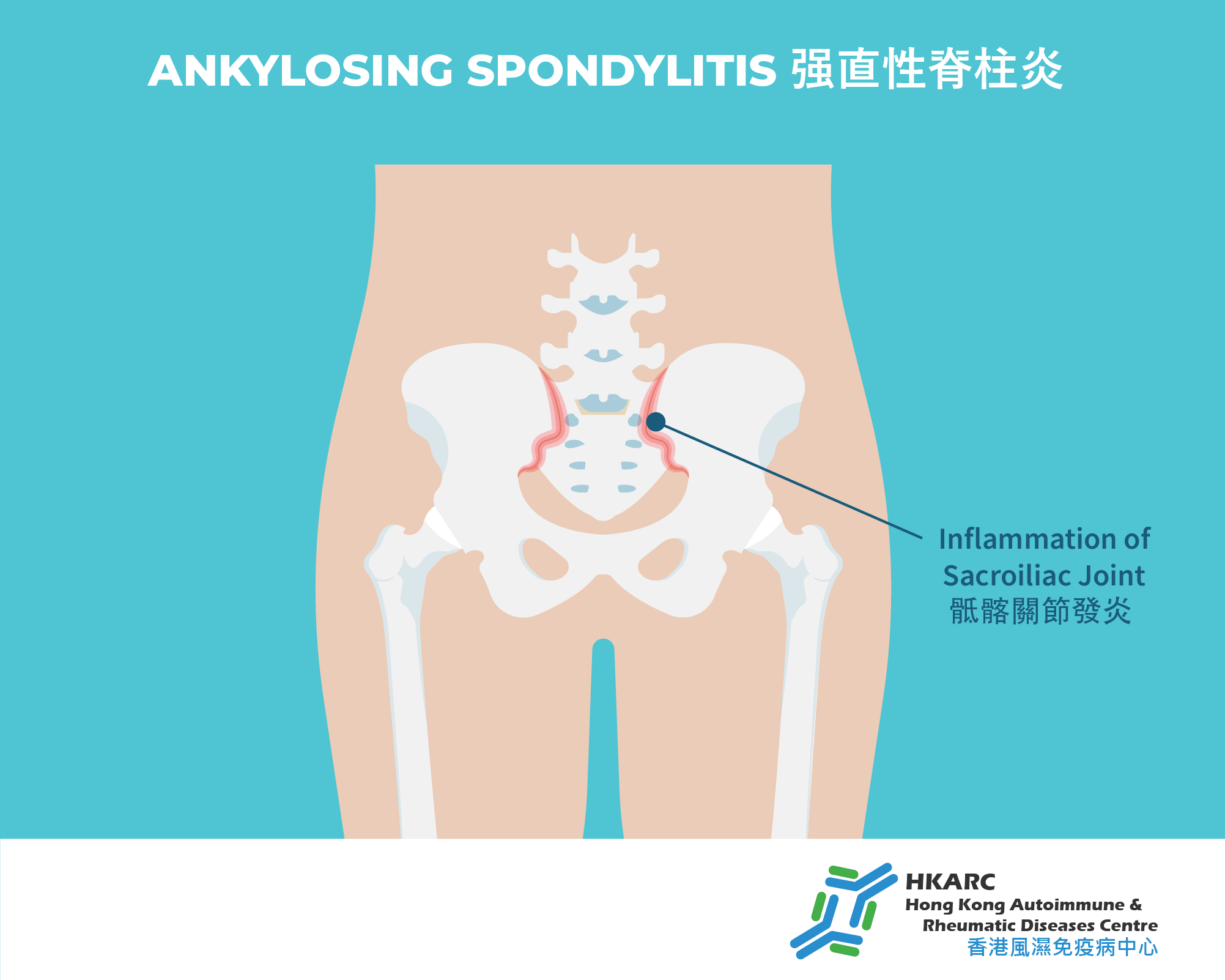
AS primarily affects the spine and sacroiliac joints. Patients typically experience inflammatory back pain lasting longer than three months. Inflammatory pain is characterized by increased pain after rest (such as upon waking), which tends to improve with activity. Long-term inflammation can lead to bone proliferation, gradually causing fusion between vertebrae, and even resulting in a bamboo spine appearance, leading to permanent spinal stiffness. Patients may find simple movements like bending forward or turning around difficult.
In addition to back pain, the sacroiliac joints and hips are common affected areas. Besides persistent pain, joint mobility may also be restricted. Some patients may develop peripheral arthritis, dactylitis (sausage digits), or enthesitis (inflammation at the attachment points of tendons and ligaments). AS patients may also experience comorbidities such as uveitis, psoriasis, and intestinal inflammation, and may have an increased risk of cardiovascular diseases.
Diagnosis of Ankylosing Spondylitis
AS has a strong genetic component. About 90% of patients carry the HLA-B27 gene. However, carrying HLA-B27 does not necessarily mean one will develop AS; only about 7% of HLA-B27 carriers develop the disease.
Diagnosis involves blood tests, X-rays, and MRI scans:
Blood Tests – primarily to detect inflammation markers and HLA-B27 antigen. Inflammatory markers include Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP), which help determine if the spine and joints are inflamed.
X-rays and MRI – used to assess inflammation and fibrosis in the sacroiliac joints and spine.
Treatment Options
Patients generally respond well to Nonsteroidal Anti-Inflammatory Drugs (NSAIDs). Some may consider traditional Disease-Modifying Anti-Rheumatic Drugs (DMARDs), but these often have limited effectiveness. Early use of biologic agents can effectively control inflammation and reduce structural damage, playing a vital role in improving quality of life and joint function.
NSAIDs
NSAIDs help reduce symptoms and inflammation, providing short-term disease control. Long-term use is not recommended due to potential side effects such as stomach pain, ulcers, renal failure, liver effects, and cardiovascular risks. COX-II inhibitors, a subclass of NSAIDs, tend to have fewer gastrointestinal side effects.
Traditional DMARDs
These can gradually replace steroids, improving immune regulation, reducing joint inflammation and destruction, alleviating pain, swelling, and stiffness, and slowing disease progression to help maintain joint function.
Biologics/Targeted Synthetic DMARDs
Used mainly for patients with high disease activity or those who do not respond well to traditional treatments. Biologics target specific immune factors such as TNF-alpha or IL-17, while targeted synthetic DMARDs (like JAK inhibitors) suppress inflammation, relieving pain and stiffness, and improving spinal mobility.
FAQs
• What are the early symptoms of Ankylosing Spondylitis?
Early symptoms include chronic pain and stiffness in the lower back and hips lasting over three months, especially noticeable in the morning or after prolonged rest. Additional symptoms may include morning stiffness, back pain, spinal rigidity, and pain or stiffness in the hips, shoulders, or knees.
• What inflammation markers are tested for AS?
Blood tests measure ESR, CRP, and HLA-B27 antigen levels, which can serve as indicators for diagnosis.
• Can blood tests alone diagnose AS?
Blood tests can provide preliminary clues but must be combined with clinical assessments and imaging studies (X-rays and MRI) to confirm inflammation and fibrosis.
BASDAI Questionnaire Score Calculator
- The Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) is a validated diagnostic test that determines the effectiveness of the current treatment for individuals who suffer from Ankylosing Spondylitis.
- If you have a score of 4 or more, you may benefit from a medical review by your rheumatologist.