What is Psoriatic Arthritis (PsA)?
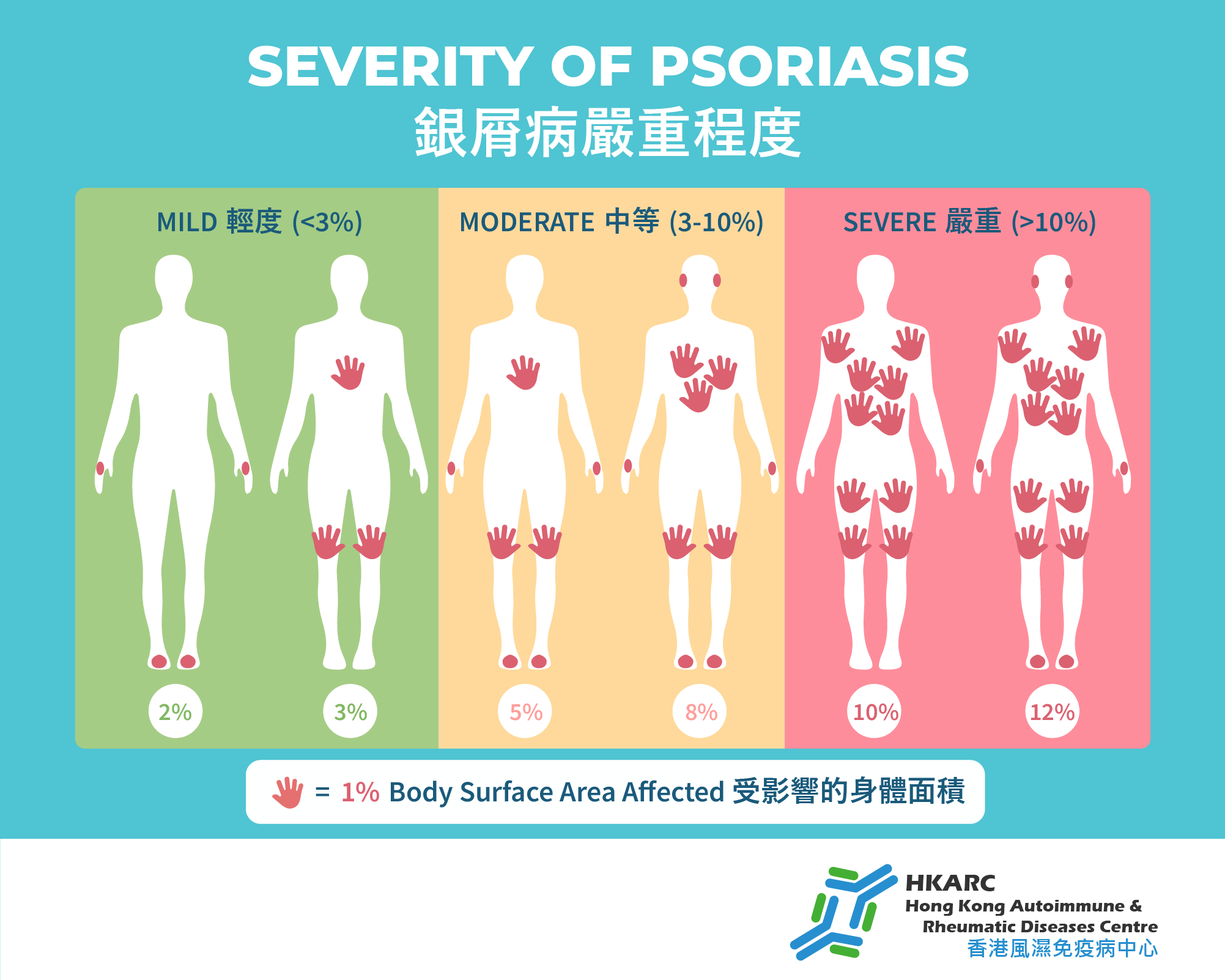
Psoriatic Arthritis is an autoimmune disease commonly known as “psoriasis-related” or “silver-scaled skin”. It results from immune system dysregulation that attacks the skin and joints. Patients develop well-defined red patches covered with silvery-white scales on various parts of the skin, often accompanied by flaking. Over time, it can cause permanent deformities.
Psoriasis-associated joint inflammation is classified into five main types:
- Symmetrical polyarthritis, mainly affecting the distal interphalangeal joints of fingers.
- Axial Spinal Arthritis, primarily involving the spine and hips.
- Distal interphalangeal joint involvement.
- Oligoarthritis – affecting fewer large joints like knees and elbows.
- Arthritis mutilans – a severe, destructive form leading to joint deformities and permanent damage.
Are Psoriasis and Psoriatic Arthritis the Same?
While both are related to psoriasis, they are not identical. Psoriasis is a skin disease characterized by red, scaly patches, commonly on the scalp, elbows, knees, and other areas. Psoriatic arthritis (PsA) is a complication where the immune system also attacks the joints, occurring in approximately 30-40% of psoriasis patients. PsA causes joint swelling, pain, stiffness, and can lead to deformities.
Symptoms of Psoriatic Arthritis:
Skin:
- Red patches with white scales
- Itching and dryness
- Nail changes such as pitting, separation, or discoloration
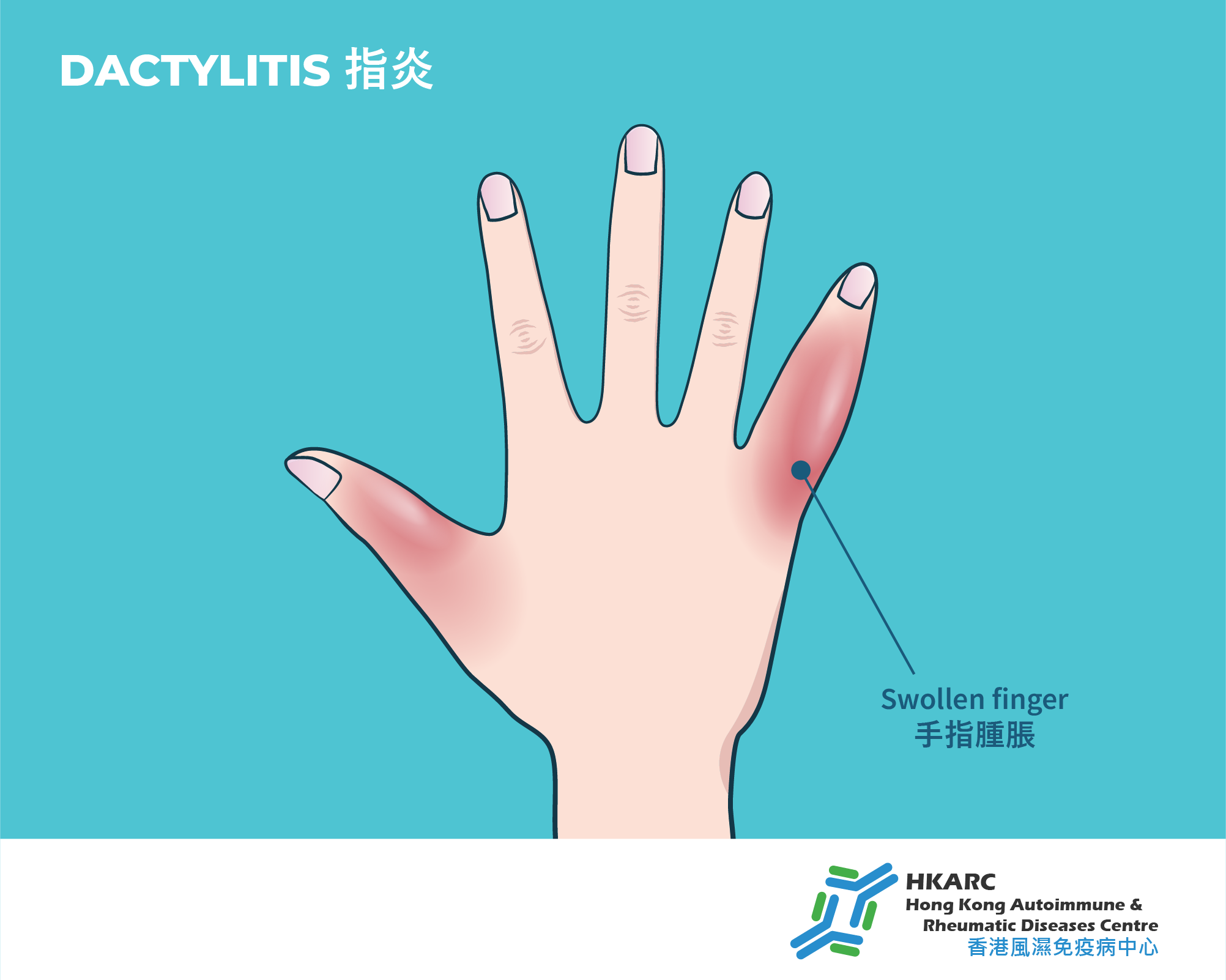
Joints:
- Pain, stiffness, or swelling
- Reduced mobility
Others:
- Fatigue
- Redness and eye pain
Impact on Patients and Comorbidities: Psoriatic arthritis can affect more than joints and skin. It is associated with other conditions like metabolic syndrome, obesity, hyperuricemia, hypertension, diabetes, dyslipidemia, and fatty liver, increasing cardiovascular risk. The visible skin and joint symptoms can also affect self-image and emotional well-being.
Treatment Options
To effectively control the disease, early use of DMARDs or biologics is recommended, which can more specifically and effectively manage symptoms and improve quality of life.
Traditional DMARDs
These can gradually replace steroids, suppress immune activity, reduce joint inflammation and destruction, and slow disease progression, helping maintain joint function.
Biologics/Targeted Synthetic DMARDs
Biologics target specific cytokines such as TNF-alpha, IL-17, or IL-23, or oral targeted drugs like JAK inhibitors. They significantly inhibit inflammation, relieving skin and joint symptoms. Due to their high specificity, they tend to have better efficacy, safety, and fewer side effects compared to traditional medications.
FAQs
• Do all psoriasis patients develop psoriatic arthritis?
Approximately 30-40% of psoriasis patients may develop psoriatic arthritis. Some patients may first experience joint symptoms before skin manifestations.
• Are there complications associated with psoriatic arthritis?
Some patients may develop uveitis or spondylitis. PsA is also associated with a higher risk of metabolic syndrome, cardiovascular disease, diabetes, hypertension, and fatty liver.
• How do biologics treat psoriatic arthritis?
Targeting key inflammatory cytokines like TNF-alpha, IL-17, and IL-23 is a major focus of recent therapies. These biologics effectively suppress inflammation, alleviating skin and joint symptoms. In particular, inhibiting IL-17/IL-23 is especially effective for controlling skin lesions.